“Few things a doctor does are more important than relieving pain… pain is soul destroying. No patient should have to endure intense pain unnecessarily. The quality of mercy is essential to the practice of medicine; here, of all places, it should not be strained.” – Marcia Angell
As a person in constant chronic pain, discussing my pain with my doctors is frustrating for two major reasons. One is that, no matter how many things they try, doctors’ attempts to alleviate my pain haven’t gotten us very far. Hearing them ask how much relief they’ve brought me with their treatments just means I have to admit to them that, despite their expertise and well-wishing, they haven’t been able to help me. I don’t want to disappoint them. I know that my illness confounds them, and I want desperately to be able to report good news. Each time I have to report that my pain hasn’t budged, I know I’m reminding them there are some things that even they can’t fix.
When I go to give doctors details about my pain, I run into my second big frustration; there is no good shorthand for expressing what my pain is like. Some doctors’ offices give me lists of adjectives for me to choose from, such as “burning,” and “stabbing.” Others ask me to rate the amount that my pain impacts my ability to carry out my daily tasks. Still others ask how much my pain is a problem for me at work.[1]These methods of getting at how much pain I’m in are all useful, but only give my doctors limited information about the pain. The most common way doctors’ offices ask me to rate my pain is from zero to ten, using the “standard ten-point pain scale.” I believe this to be the least effective tool that doctors use to learn about my pain, because it is exceptionally flawed[2] and hard to use.
My major issue with the “standard ten-point pain scale” is that it lacks a standardized meaning. I’ve never known what to make of the smiley-face version of this pain scale, and I’ve heard enough complaints about it from other patients and other internet users to know I’m not alone. The most common way that doctors talk about this scale is, “Tell me your pain level on a scale from 0 to 10, where 0 means no pain, and 10 means the worst pain imaginable.” Well, I have a pretty vivid imagination, so when I broke my foot a few years back, I reported my pain as a 3 on the pain scale. This pain was bad enough to keep me from sleeping, and to make me cry if I accidentally put my full weight on the foot. However, I figured that what I was experiencing was probably 30% of what awful, deathly, torturous pain would feel like. Using that same perspective, for the first few months after I got really sick in 2012, I was reporting my migraine/body pain levels as being between 3 and 4. My boyfriend was convinced that my estimate was too conservative, and he proved himself right by finding me my first pain scale with helpful text written out about each pain level. I saw pain between 3 and 5 described as “low intensity” and pain between 6 and 7 described as “miserable.” I had been miserable and in severe pain for months, while reporting low intensity pain. It was clear that I had been failing to communicate the severity of my pain to my doctors, and that this was because the standard ten-point pain scale is way too open to interpretation[3].
Luckily, I have found a tool which is much more helpful. A couple of months ago, I participated in a webinar about how healthcare providers can help manage their patients’ pain during hospitalization (The full webinar is available here, or you can access just the slides.). I found the talk to have a handful of good tips that I as a healthcare professional hadn’t previously considered. As a patient, though, I was exceptionally grateful that I had tuned in, because I came away from the webinar with exposure to the exceptionally useful comparative pain scale from the Children’s Hospital at Stanford.
I want to share this pain scale with all of my friends and family, my colleagues, and all of my caregivers. I want this to be the starting place that every US healthcare provider uses to ask their patients questions about their pain. Patients using this tool with their healthcare providers could trust that their experiences with pain would be thoroughly and efficiently communicated.
When I say that for the majority of my days I’m at a 7 on the pain scale, I want my doctors to understand that my pain is strong, deep, piercing, and dominates my senses. I want them to have an understanding of how this level of pain would feel, and with this pain scale I think they would, given the comparisons the scale makes to other familiar types of pain. I also want them to understand the impact that this kind of pain has on my ability to “be normal.” This scale would help with that, and it even includes some insight into what toll this level of pain will take when experienced long-term. This scale has it all.
If patients and doctors could move from using the standard ten-point pain scale to the Stanford comparative pain scale, a huge amount of mystery would be taken out of our conversations. There would still be patients who exaggerated their pain, or underreported it. By and large, though, doctors would have a much-improved handle on the extent to which their patients were suffering, and a better understanding of which treatments gave what amount of relief. Selfishly, I want all of my doctors to be conversant in this pain scale, so we can have one less obstacle in our work together to fight my chronic pain.
[1] This question is particularly hard to hear repeatedly from the same healthcare providers, since I expect them to remember that I’ve been unable to work for a year and a half.
[2] My first issue with the “standard ten-point pain scale” is a pedantic issue, and the fact that I can’t just let it go demonstrates that I’m a major nerd. See, a scale where I can report “no pain” as zero, or I can report increasing amounts of pain by using any number from one to ten is an eleven-point scale.
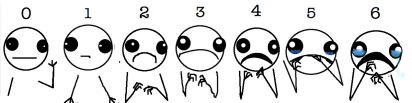
[3] Perhaps a lot of this type of confusion could be avoided if the “standard ten-point pain scale” were depicted more graphically, as it is when redrawn in a post on Hyperbole and a Half:


Pingback: Rethinking the Traditional Pain Scale | The Professional Patient
I am one who hates when asked to rate your pain on a scale of 1-10 when you go to the E.R. or in a doctors office. With chronic pain sufferers it is not that easy to do. It’s very annoying most of the time because you feel that they just don’t get it. For patients that are supposed to be less stressed, this is what stresses them.
I hear you! The fact that certain answers will make us be seen as exaggerators and certain answers will be too conservative to have our complaints taken seriously makes this a very stressful question indeed.
Pingback: The Challenges of Doctor-Patient Communication About Pain, and a Tool That Could Help | RainCloudMom's World